What we know.
Three professional perspectives on the pandemic’s impact on our sleep—including tips on how to sleep better.
From the Taskforce
Associate Professor Sutapa Mukherjee of Flinders University has been a sleep physician since 2005. In addition to working as a sleep physician at SA Health in Adelaide, Australia, this year she added a new title: Co-Chair of the Guideline Leadership Group of the National COVID-19 Clinical Evidence Taskforce of Australia (covid19evidence.net.au).

AUSTRALIA’S COVID-19 SLEEP RESEARCH
In Dr. Mukherjee’s role as President-elect of the Australasian Sleep Association, she has been part of a group monitoring the impact of COVID-19 on sleep in patients and colleagues, as well as following international and national literature as it becomes available.
“Anecdotally, many of us observed major changes in our own sleep patterns. Definitely routines have changed, particularly during the early stages of lockdown in Australia (March-April) when many people were working from home. This had positive effects on some patients because they could sleep when they pleased rather than being tied down to a work schedule. Also, there was no work commuting time so they could go to bed later and get out of bed later and still be on time for work. This particularly suited the ‘night owls’ who often struggle to get out of bed in the morning. Overall, people were in bed more,” Dr. Mukherjee explains.
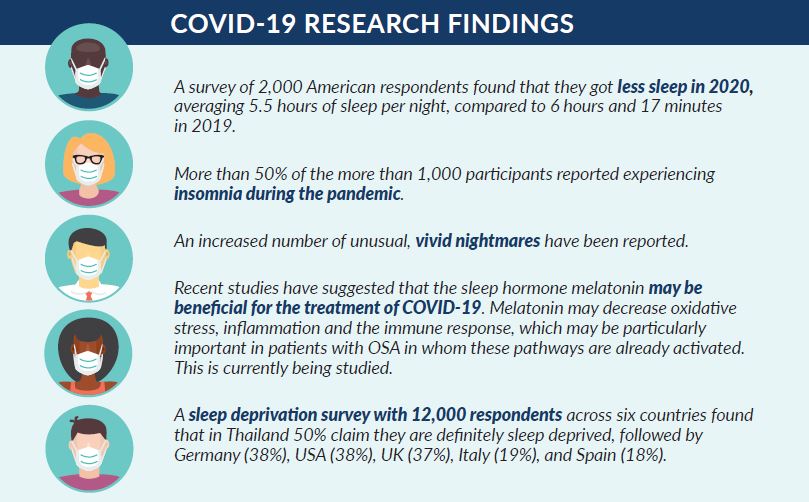
Yet as time wore on during the pandemic, Dr. Mukherjee and her colleagues began to notice more patients overall reporting poor sleep, especially in those who were previously good sleepers. “There was definitely more anxiety,” Dr. Mukherjee observed. “And watching the news and social media as the pandemic developed led many to worry, often resulting in increased difficulty falling asleep or staying asleep.” Dr. Mukherjee and her colleagues often noted patients reporting more vivid dreams, increased stress, less exercise and sunlight (both of which help to regulate sleep) and more time using electronic devices before bed.
WHAT IS KNOWN ABOUT SLEEP IN PATIENTS WITH COVID-19
Dr. Mukherjee explains that there is some evidence that patients with sleep apnea may have more severe symptoms. “Emerging research suggests that sleep apnea might be a risk factor for more severe disease and COVID-19 Mortality and Hospitalization. “Otherwise, not much is known about those recovering sleep patterns, apart from some who seem to feel very fatigued and spend more time in bed. At this point, we know very little, and I am sure this will be an active area of research in the future.”
DR. MUKHERJEE’S SLEEP TIPS
• Remember it is normal to feel anxious and overwhelmed with the current situation
• Stick to a set routine each day
• Allow downtime for relaxation and unwinding before sleep
• Avoid screentime before bed
• Stay in contact with others and keep up your social connections even though you may not be able to meet face to face
• Be mindful/meditate
• Exercise and stick to a healthy diet
• Take a short nap if you are very tired, around 20 minutes, but not after 3pm
• Avoid caffeine after midday.
From the Physician

Dr. Hari Wimaleswaran, MBBS, B.Physio, CCPU, FRACP is a Consultant Respiratory and Sleep Medicine Physician at Austin Health, Monash Health, Cabrini Health and Warringal Private Hospital in Victoria, Australia. As of May 2020, he also became the Respiratory Clinical Lead for the management of COVID-19 positive patients and outpatient followups. Since its inception, the group has been reviewing complications and long-term outcomes of COVID-19—the first of its kind in Australia. In assessing the patients over time and being up-to-date with emerging and evolving medical literature covering COVID-19, sleep disturbances such as insomnia and non-restorative sleep have become apparent. Dr. Wimaleswaran states, “Sleep disturbances were evident in the SARS epidemic and persisted for up to two years. There is mounting evidence that it has also become a strong signal in the COVID-19 pandemic.
Traditional risk factors of poor sleep including inactivity, anxiety and depression have been further intensified during the COVID-19 climate leading to a further decline.” Findings suggest that sleep disorders have been reported in approximately 31% of COVID-19 patients. “In our experience,” Dr. Wimaleswaran begins, “nearly 30% of patients that were evaluated showed signs of insomnia at 8 weeks post-infection. In particular, healthcare workers were especially at higher risk for insomnia. This subgroup is not entirely surprising given the provision of care to patients, fear of being infected and witnessing death firsthand on accounts.”
Dr. Wimaleswaran is quick to note that sleep disturbances such as insomnia are a normal reaction to stressful events, including COVID-19. Especially considering we have all been affected in some way or another. “The confinement indoors and the severe disruption in routine have been big players in sleep disturbance,” Dr. Wimaleswaran continues. “When we lose certain life ‘prompts’ during the day for the body such as meal times, activities and sleep, the circadian rhythm is prone to disruption. The key is to normalize this as best as possible. I wish for people to take comfort in knowing sleep issues during COVID-19 are an appropriate response by the body.”
From the Psychologist
Dr. Melinda L. Jackson is Senior lecturer and Psychologist at Turner Institute for Brain and Mental Health, Monash University in Australia. She has been working in the field of sleep for 15 years.

Her team of sleep psychologists were keen to find out how the pandemic is impacting people’s sleep-wake patterns and psychological functioning. They conducted a global survey on sleep and mental health during the early stages of the pandemic (March-April) and have followed people up over the last six months.
CHANGES IN SLEEP
“At first,” Dr. Jackson began, “we thought the psychological impact of the uncertainty and fear of infection would be the main influence on sleep. We later realized the stay-at-home orders and enormous changes to day-to-day lives and routines had a significant impact as well. Our survey aimed to look at whether particular factors—such as resilience, personality, loneliness—may be protective for sleep, or in fact, detrimental.”
The team discovered a division in how people responded to the COVID-19 situation, in terms of their sleep and wake patterns. Dr. Jackson states, “We found that 73% of respondents met criteria for poor sleep quality based on the Pittsburgh Sleep Quality Index during the March-April period. This is not surprising, since we know that stress is a major precipitant of insomnia, and a global stressful event like a pandemic is bound to bring out sleep problems in some people.” But the team also found that some people reported sleeping better. This may be because people did not have to wake up early to get to school or work, and therefore could go to bed and wake up at a time that suited their own internal body clocks. “Around half of our respondents indicated that their sleep was in better alignment with their body clock compared to before the pandemic,” Dr. Jackson explains.
“This is similar to other reports from Europe and the US. The pandemic has brought about a naturalistic experiment to see what happens when we’re not dictated by what our work or schooling schedules require us to do. These findings suggest that when people are allowed to sleep on their own time, people will potentially get more sleep and sleep on schedule that better aligns with their body clocks.”
SLEEP AFTER A POSITIVE TEST
Dr. Jackson and her team are also aware of the emerging evidence suggesting that those who have been infected with COVID-19 experience anxiety and poor sleep quality, perhaps due to the impact of isolation and hospitalization. Dr. Jackson notes that one of the symptoms of long haul COVID includes insomnia. “Strong immunity often begins with good sleep. We should not underestimate the importance of good sleep for immunity,” Dr. Jackson concludes.
……………………………………………….
Gina Dewink has been working and writing for nonprofit health organizations since 2004. With a degree in communications, her career history includes the American Academy of Neurology and the RLS Foundation.
References
Am J Respir Crit Care Med. 2020 Nov 15; 202(10): 1462–1464. Published online 2020 Nov 15. doi: 10.1164/rccm.202006-2252LE PMCID: PMC7667903 PMID: 32946275
Sleep Apnea and COVID-19 Mortality and Hospitalization. Brian E. Cade,1,2, * Hassan S. Dashti,2,4,5 Syed M. Hassan,1,2 Susan Redline,1,2,6 and Elizabeth W. Karlson1,2,3
Further Reading on the topic (links not affiliated)



